Persistence, passion lead to new attack on parasitic diseases
Wednesday 25 July 2012
Based on research by UCSF and UC San Diego, the FDA has identified an arthritis treatment as an “orphan drug.” It paves the way for a new drug to attack tropical parasites that disable and kill millions of people worldwide.
Passion, inventiveness and good luck have led UC scientists to a new use for an old drug. The discovery promises to protect millions of people and save thousands of lives.
For more than 20 years, a group of UCSF and UC San Diego researchers have been on the trail of drugs to kill pernicious tropical parasites that drug companies don’t pursue.
Last year, they hit gold. They showed in lab and animal studies that an arthritis drug called auranofin can knock out a particularly aggressive parasite that disables hundreds of thousands and kills 70,000 people a year. The drug also cripples a second protozoan parasite responsible for nearly 300 million infections a year.
Auranofin has been on the market since 1985, and its safety is well established. So, the time and cost needed to develop it to treat the infectious diseases should be greatly reduced.
What’s more the UC researchers have already shown that auranofin is far more potent than the best drug currently used against the tropical infections — an antibiotic called metronidazole, known to cause side effects such as nausea, vomiting and dizziness. If clinical trials confirm its effectiveness in infected people, the arthritis drug could be used at a lower dose and at a much lower cost per person, they said.
Effective, safe and potent: So far, it’s a win-win-win. Overcoming the safety hurdle at the outset “moves us much closer to our goal of a more effective drug to treat these devastating diseases and infections,” said Jim McKerrow, professor of pathology in the UCSF Center for Discovery and Innovation in Parasitic Diseases and one of the leaders in the discovery.
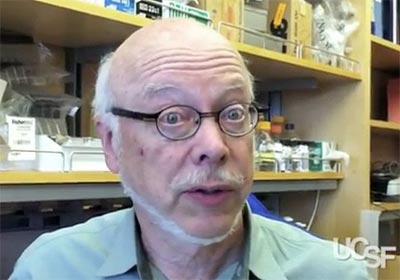 McKerrow has committed his career to finding drugs to treat
neglected diseases of the developing world.
He is an expert on the role of certain enzymes in parasites and in the
search for drugs to disrupt the enzymes to cripple the pathogens.
McKerrow has committed his career to finding drugs to treat
neglected diseases of the developing world.
He is an expert on the role of certain enzymes in parasites and in the
search for drugs to disrupt the enzymes to cripple the pathogens.
Co-leader in the new research is Sharon Reed, professor of pathology and medicine at UC San Diego, who shares a lifelong pursuit of finding treatments for parasitic diseases. She and McKerrow have collaborated on at least four major research projects aimed at finding causes of and treating debilitating parasitic diseases.
“My main mission over more than 25 years has been to further the understanding of how parasites cause infection,” she said. “Working with Jim, it has been very exciting to see these findings lead to potential new drugs.”
Based on the team’s research, the FDA has now officially identified auranofin as an “orphan drug,” recognizing its new potential to treat diseases that pharmaceutical companies don’t target normally because of poor prospects for profit.
The researchers now have applied for approval and funding to launch clinical trials as early as next year to test the drug in people infected by either of the two parasites.
One parasite, called Entamoeba histolytica, causes amoebiasis, a spectrum of diseases ranging from diarrhea to severe intestinal inflammation, known as colitis. In some cases, it leads to infection in other organs. It is the source of more intestinal disease than any other parasite in the world. The other protozoan, Giardia lamblia, is less severe, but also causes chronic diarrhea. It often targets children in tropical countries, as well as nearly 20,000 people in the U.S due to contaminated water or fecal contact.
The discovery stems from both a serendipitous event and a new strategy to screen drugs against organisms that live in the oxygen-free environment of the gut.
The team had the good fortune to be offered a library of some 900 FDA-approved drugs — known bioactive compounds — licensed by the biotech company Iconix Biosciences, which was going out of business. The company chose to offer the drugs to McKerrow and the UCSF center because of the unit’s reputation for identifying molecular interactions underlying parasite metabolism and finding drugs to exploit them.
McKerrow’s team worked with the Small Molecule Discovery Center at UCSF to screen the drugs against the protozoan parasites in culture. Auranofin was the top “hit” from the Iconix library. It turned out that auranofin was 10 times more potent against E. histolytica than is metranidazole.
“We were startled,” McKerrow says. “And we were excited because we knew auranofin could be safely taken orally. We were already a giant step ahead.”
Screening drugs against the parasites posed a unique problem. Infectious organisms that live in the gut can’t be tested in the efficient high-volume process known as high-throughput screening. This method normally allows hundreds or thousands of promising compounds to be tested at once. But until now, drugs against anaerobic pathogens had to be tested a few at a time.
Anjan Debnath, a UCSF postdoctoral scientist in the center, developed an automated screen that could be conducted in anaerobic conditions, and coupled it with an effective way to compare different drug’s success at blocking the action of an enzyme the scientists suspected was essential for the parasite’s survival.
Once the UCSF team had established the drug’s success in the lab, UC San Diego and Mexico research partners began experiments to test the drug’s success in infected animals. Reed’s UC San Diego team had already developed a way to study amoebiais in mice, and colleagues in Mexico had perfected a hamster model to study the amoeba in the liver. Both groups found that auranofin was the most potent drug they had ever tested against the pathogen.
McKerrow’s and Reed’s labs have since worked with scientists at the Wake Forest School of Medicine to show specifically how the drug kills parasites. It inhibits an enzyme the parasites need to protect themselves against attack by the host immune system. A molecular model of how that happens was solved by UCSF crystallographer Larissa Podust.
Research now suggests that other parasites, such as Trichomonas and Brugia, also might be vulnerable to auranofin. McKerrow and Reed hope to confirm its potential against the other diseases.
“This discovery validates the idea that ‘repurposing’ existing drugs can overcome many of the challenges inherent in developing treatments for neglected diseases,” said McKerrow.
The research was supported by the Sandler Foundation and the National Institute of Allergy and Infectious Diseases.